公司资讯
13
Apr

0
July,4th, 2019 sunny
Definition of special nouns
Abandoned cycle with IVF / ICSI
Prior to egg retrieval, usually due to a lack of response (where fewer than three mature follicles are present) or conversely if there has been an excessive response to gonadotrophins and the patient is at risk of severe ovarian hyperstimulation syndrome (OHSS). One abandoned cycle does not count towards the number of commissioned cycles.
Assisted reproduction
The collective name for treatments designed to lead to conception by means other than sexual intercourse, which include intrauterine insemination (IUI), in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI) and donor insemination (DI).
Blastocyst
Blastocyst stage embryos are selected on day five of their development (or on day six if they have not developed by day five).
Cleavage
Cleavage stage embryos are selected on day one or day two of their development
Clinical pregnancy
A pregnancy diagnosed by ultrasonographic visualization of one or more gestational sacs. It includes ectopic pregnancy. Note: multiple gestational sacs are counted as one clinical pregnancy.
Cryopreservation
The freezing and storage of embryos, sperm or eggs for future use in IVF treatment cycles.
Donor insemination
DI is a type of fertility treatment in which high quality donor sperm is used when either the male partner has no sperm or for lesbian couples. This sperm is then injected directly into the womb (IUI).
Embryo transfer
The procedure in which one or more embryos are placed in the uterus.
Fertilisation
The union of an egg and sperm.
Full cycle
This term is used to define a full IVF treatment, comprising of one episode of ovarian stimulation and the transfer of any resultant fresh embryo(s). Where an excess of embryos is available following a fresh cycle, these embryos may be frozen for future use. Once thawed, these embryos may be transferred to the patient as a frozen cycle and be included within the ‘full cycle’.
All frozen embryos from a previous cycle should be used before a further IVF cycle is initiated.
Storage of frozen embryos will be routinely funded for one year unless the provider has agreed an alternative as part of a pathway agreement.
July,8th, 2019 cloudy
Egg freezing in numbers:
1310 egg freezing cycles in 2016
18% birth rate from frozen own eggs
519 egg thaw treatment cycles in 2016
156 babies born from frozen eggs in 2016
0.8% of all IVF cycles are egg freezing cycles
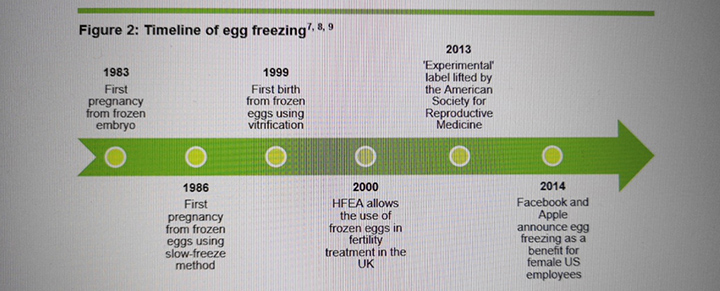
1999 first birth from frozen eggs using vitrification method
30% birth rate from frozen donor eggs
10253 eggs stored in 2016
July,9th, 2019 cloudy
Key factors to consider about egg freezing:
The number of egg freezing cycles has increased each year since 1999 and more than doubled since 2013.
The age at which eggs are frozen
The chances of success alongside risks
The 10-year limit on storing frozen eggs
Cost-a full cycle of freezing and thawing eggs is 7000-8000.
35-most common age to have IVF
38-most common age to freeze eggs
40-most common age to thaw own eggs
July,10th, 2019 fine
The UK legal framework for egg freezing All fertility clinics in the UK must comply with the Human Fertilisation and Embryology (HFE) Act 1990 (as amended), the HFE Act 2008, and a number of related pieces of legislation. Freezing eggs can be carried out by any clinic provided they have a licence from us to do so. The law sets out that the standard storage period for eggs and sperm is 10 years. After 10 years, any eggs that a patient still has frozen must be destroyed. There is the option to extend storage to 55 years, when patients are, or likely to become, prematurely infertile. The diagnosis for premature infertility must be made by a written statement from a medical practitioner.
July,11th, 2019 fine
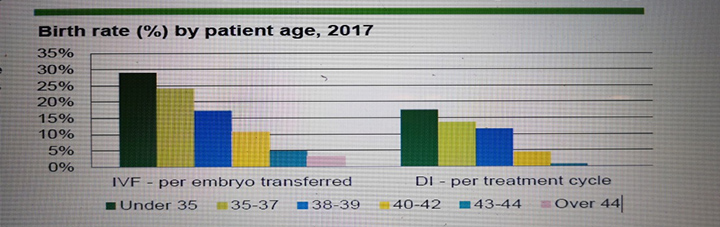
The impact of donor eggs on success rates In 2016, donor eggs overall had a significantly higher success rate per thaw treatment cycle (30%) than own eggs (18%). As noted earlier, the significantly higher success rates for donor eggs compared to own eggs is to be expected and is largely due to the access criteria applied to women who donate their eggs. This access criteria requires women to have healthy indications for fertility, such as BMI, age and lifestyle factors.
July,12th, 2019 cloudy
The costs of egg freezing and thawing NHS funded The National Institute for Health and Care Excellence (NICE) recommends that women who are diagnosed with cancer that is likely to affect their fertility should be offered fertility preservation on the NHS. Fertility preservation could include embryo or egg storage, depending on which is most appropriate. When women who have preserved their fertility due to medical reasons then wish to use their frozen eggs, they would be eligible for NHS funding for treatment. Privately funded A review of prices advertised on UK clinic websites in May 2018 showed that the average cost of a complete egg freezing cycle, including storage and use of eggs in future treatment, ranges from £7,000-£8,000. This is made up of the cost of egg freezing, storage and using frozen eggs in treatment. Prices range from £2,720-£3,920 for an egg freezing cycle, with the average (median) cost for freezing eggs being around £3,350. There are variations in what is included within this cost, with most clinics including one or two years of storage. However, these costs do not include the medication required for treatment which can vary from £500 to thousands. The cost of storing eggs also ranges from £125-£350 a year. When it comes to using frozen eggs in treatment, costs range from £1,650-£4000, with the average (median) being around £2,500. Freezing eggs is therefore a significant investment and, as with all fertility treatment, clinics should inform patients of all the relevant costs upfront, so they have an accurate idea of how much the full process is likely to be.
July,15th, 2019 cloudy
Something about the consent form related to reproductive center
Your consent to extending the storage of your embryos beyond 10 years.
This form is produced by the Human Fertilisation and Embryology Authority (HFEA), the UK’s independent regulator of fertility treatment and human embryo research. For more information about us, visit www.hfea.gov.uk.
l Who should fill in this form?
Fill in this form if you already have embryos in storage (created outside the body (in vitro) using your sperm or eggs) and wish to extend your current storage period beyond 10 years. By law, you can only do this if you, your partner, or the person to whom your embryos have been allocated, are, or are likely to become, prematurely infertile. Your clinic will need to attach a medical practitioner’s statement confirming this to this form.
Please do not complete this form if you are:
storing your embryos for the first time
changing the period for which you consented to store them within the 10 year standard storage period. Instead you should revise the storage period on the original form by completing another copy of that form.
l You must also state in writing how long you consent to your embryos remaining in storage. How long can I extend storage by?
Providing you, your partner, or the person to whom your embryos have been allocated, meet the medical criteria for premature infertility, you can consent to store your embryos for up to 55 years. If you have your embryos in storage and wish to extend storage beyond 10 years, a medical practitioner will need to certify in writing that you or your partner has met the medical criteria for premature infertility for storage to continue.
July,16th, 2019 cloudy
Is the surrogate married or in a civil partnership?
The husband or civil partner will be the legal father or parent of any child born as a result of her treatment, unless: (a) the surrogate and her husband or civil partner were judicially separated at the time of the treatment, or (b) it is shown, ‘as a question of fact’ (see box 6H), that her husband or civil partner did not consent to her treatment.
Has both the intended father provided sperm and the intended female parent provided eggs for the surrogacy treatment?
The intended father can be the legal father at common law when the child is born (if no one else has been nominated). Or The intended female parent can be the legal parent when the child is born if: (a) both she and the surrogate have given the relevant consent (b) neither consent has been withdrawn (or superseded), and (c) they are not within prohibited degrees of relationship to each other.
July,17th, 2019 cloudy
l Has donor sperm and the intended female parent’s eggs been used for the surrogacy treatment?
The intended father can be the legal father when the child is born if: (a) both he and the surrogate have given the relevant consent (b) neither consent has been withdrawn (or superseded), and (c) they are not within prohibited degrees of relationship to each other. Or The intended female parent can be the legal parent when the child is born if: (a) both she and the surrogate have given the relevant consent (b) neither consent has been withdrawn (or superseded), and (c) they are not within prohibited degrees of relationship to each other.
l Have donor eggs (or the surrogate’s eggs) and the intended father’s sperm been used for the surrogacy treatment?
The intended father can be the legal father at common law when the child is born (if no one else has been nominated). Or The intended female parent can be the legal parent when the child is born if: (a) both she and the surrogate have given the relevant consent (b) neither consent has been withdrawn (or superseded), and (c) they are not within prohibited degrees of relationship to each other.